Visual Field Testing
 Although the test can be used to detect defects caused by various medical conditions such as stroke, brain tumors or other neurological deficits, it is most frequently used in eye care practices to diagnose, monitor or rule out glaucoma.
Although the test can be used to detect defects caused by various medical conditions such as stroke, brain tumors or other neurological deficits, it is most frequently used in eye care practices to diagnose, monitor or rule out glaucoma.
The visual field test is carried out by a computerized machine, called a Humphrey™ Field Analyzer, but other systems are currently used as well. The results are printed out and the doctor discusses the results with you. Occasionally, the test has to be repeated when results are uncertain.
The test primarily measures the quality and quantity of peripheral or “side” vision you have. It is a straightforward and painless test which does not involve eye drops. Essentially, lights are flashed on and you have to press a button whenever you see the light. Your head is kept still on a chin rest. The lights are bright or dim at different stages of the test. Some of the flashes are to check if you are concentrating. Each eye is tested separately and the entire test takes less than 20 minutes.
Digital Retinal Imaging
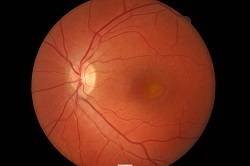 Digital photography has revolutionized the camera industry and it has also revolutionized healthcare.
Digital photography has revolutionized the camera industry and it has also revolutionized healthcare.
Digital Retinal Imaging is a process in which a high-resolution digital photograph is taken of the back interior portion of your eye called the retina. In most cases, the digital color image can be obtained without dilating your pupils. The image produced shows the optic nerve, blood vessels, nerve fiber layer and the macula, which is the most sensitive part of the retina and is responsible for the most clear and detailed vision you have.
The imaging can show abnormalities like tumors, hypertension, macular degeneration and diabetic retinopathy that may threaten normal vision. It also provides invaluable baseline information to assist your doctor in determining if any changes in the health of your eye have occurred from one exam to the next.
The digital imaging becomes part of your permanent record so that your doctor can closely monitor even the slightest progression of any abnormalities. You will be given the opportunity to see the images and get a thorough explanation of the images.
Topcon Maestro OCT
 The health of your eyes matters to you and it matters to us too, which is why we are offering OCT (Ocular Coherent Tomography) to all our patients. In many cases it is covered by insurance.
The health of your eyes matters to you and it matters to us too, which is why we are offering OCT (Ocular Coherent Tomography) to all our patients. In many cases it is covered by insurance.
OCT is a new, highly advanced imaging system that checks for potentially serious conditions such as glaucoma, diabetes, age-related macular degeneration, vitreous detachments and more.
Using the Topcon state-of-the-art Maestro 3-D OCT camera, your doctor will take both a digital photograph and a three dimensional cross sectional scan of the back of your eye in one sitting. This allows both instant and early diagnosis of a number of common ocular conditions. The scan is non-invasive, painless, simple, quick and comfortable. You may not need to have to have your pupils dilated. Total exam time usually takes less than a minute, and the system creates easy-to-read color images that your doctor can quickly analyze.
The software automatically detects even the most subtle changes to the retina with every eye exam you have. This gives you an invaluable ongoing record of the health and condition of your eyes. Common conditions identified through regular OCT screening include:
- Age-related macular degeneration (AMD) – AMD is a leading cause of blindness in the elderly. The OCT can help identify the earliest signs of AMD, determine whether it is the dry or wet form and help monitor its progress over time.
- Diabetes – Diabetic retinopathy is the leading cause of blindness in people of working age within the USA. OCT examination helps enable early detection of diabetic retinopathy, allowing early referral and management which can greatly improve the success rate of treatment.
- Glaucoma – Glaucoma is a condition which causes damage to the optic nerve – the part of the eye which connects to the brain – and causes gradual loss in peripheral vision. Because the early stages of chronic glaucoma do not cause symptoms, regular eye examinations are essential to detect glaucoma at its earliest stage so that ongoing damage can be prevented. OCT examination can measure numerous features at the back of the eye and facilitate early diagnosis of glaucoma.
- Vitreous detachments – Vitreomacular traction can be easily diagnosed through OCT. As we age, the vitreous jelly can shrink and cause ‘pulling’ of the retinal surface. The danger of a vitreous detachment is that there is no pain and your eyesight will seem unchanged but the back of your eye may become damaged.
- Macular holes – A macular hole is a small hole in the macula – the part of the retina which is responsible for our sharp, detailed central vision. Macular holes usually form during a complicated vitreous detachment, when the vitreous pulls away from the back of the eye, causing a hole to form. Management of this condition needs to be carried out by a retinal specialist. The OCT can easily detect macular holes at any stage.
Marco M3
Probably one of the most amazing pieces of equipment we have is our Marco M3 machine. The M3 is the world’s first and only pre-testing machine to incorporate three machines in one, hence then name M3.
The M3 has a built in auto-refractor which a computer that uses infrared beams to help determine your eyeglass prescription, it has a built in auto-keratometer which measures the curvature of your corneas which is essential in fitting contact lenses and doing laser surgery and has a built-in tonometer which is the “puff of air” test that measures the pressure of fluid inside your eyes.
Glaucoma is a disease where the eye pressure gets too high and may cause blindness.
The good news for those who have had the air puff test before is that the M3 has a new softer, gentler puff.
Sonogage Ultrasound Pachometer
A pachometer is a medical device used to measure the thickness of the cornea.
As part of our evaluation for glaucoma at Valentine Eye Care, we may use a device called the Sonogage Corneo-Gage Plus™ to obtain a painless computerized measurement of the thickness of the cornea.
In combination with other testing, corneal pachymetry can help us determine whether or not you have glaucoma as the accuracy of eye pressure measurements can be influenced by corneal thickness.
Pachymetry also has a number of other uses in comprehensive optometric care.
It can be used in the screening of keratoconus, a progressive corneal condition and is extremely important in determining whether laser eye surgery such as LASIK is suitable for a patient. Pachymetry allows us to determine if a patient has enough corneal tissue to safely have laser surgery.
Measuring corneal thickness with ultrasound is quick and easy. A numbing drop is placed in both eyes. A pen-sized probe is then used to briefly touch the surface of each eye.


